Team:WITS-South Africa/The Problem
From 2010.igem.org

http://home.ncifcrf.gov/ccr/flowcore/cervical_cancer_ribbon4.GIF
[http://www.cansa.org.za/cgi-bin/giga.cgi?cat=1313&limit=10&page=0&sort=D&cause_id=1056&cmd=cause_dir_news To find out more about HPV and cervical cancer click here!]
The Problem
Public enemy: Human Papillomavirus-induced disease
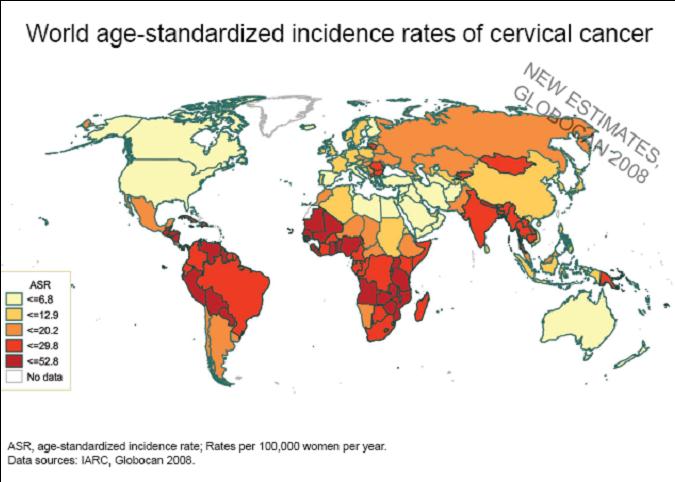
Cervical cancer is the second most prevalent cancer in women worldwide and the ause of 250 000 deaths every year. Human Papillomavirus (HPV) has been established as the etiological agent of cervical cancer - in 100% of cases of cervical cancer, HPV DNA is present.HPV is a sexually transmitted infection – in fact it is the most common STI in the world! Its ubiquity is due to the fact that it is mainly asymptomatic in men and its effects are only seen long after initial infection in women.
So what is HPV? And how does it cause disease?
HPV is a ds DNA virus which is highly host and tissue specific. It infects non-keratinised, stratified squamous epithelium (mucosal skin cells with a high rate of cellular turnover. Over 100 strains of the virus exist, some of which have been implicated in 100% cervical cancer (high-risk strains such as type 16 and 18) or cancers of the vulva, vagina, penis, anus, and head and neck (tongue, tonsils and throat).Other strains cause infectious but benign genital warts.
In most cases of infection, the body’s immune system recognises the infection and is able to clear it effectively. Most women who have been infected with HPV will never even realise it.However, HPV has developed methods of evading the immune system, including decreased antigen presentation and blunting of the interferon response. In some individuals, this results in the progression of cancer. Immunocompromised individuals are much more likely to be susceptible and risk factors such as smoking and fertility rate also contribute.
Let’s talk about South Africa…
HPV is especially problematic in the developing world where access to regular health care is limited, such as South Africa In South Africa current estimates indicate that every year 5743 women are diagnosed with cervical cancer and 3027 die from the disease. About 21% of women in the general population are estimated to harbour cervical HPV infection at a given time Early detection and careful monitoring of disease progression is vital and this is often not possible for women living in rural or under resourced areas. WHO guidelines recommend that all women aged 18 – 69 have a pap smear every three years. Only 13.6% of women in South Africa are being screened for cervical cancer according to these guidelines! Click Media:Wits_who.pdf to download the WHO fact sheet on cervical cancer in South Africa.
Detection and diagnosis
There is no antiviral or cure for HPV infection. The only diagnostic for HPV does not detect the virus itself and will only detect an infection if it has actually progressed to cancer! This is the PAP smear - a histological investigation which looks for abnormal cell morphology which arise long after the initial HPV infection as a result of virally-induced oncogenic events. A smear can detect the pathology very (too) late. PCR can also be used to detect viral DNA – this is the current gold standard for HPV diagnosis but is strain specific and impractical to implement on a wide scale at this point.
 "
"