Team:Imperial College London/Human Practices/Meetings
From 2010.igem.org
| Human Practices | Overview | Panel | Workshop | Meetings | Report | Documentary |
| Human practices has been a hugely important influence in the design of our final product. We contacted a number of experts very early on in the design process to allow us to truly adapt our specifications to meet the requirements of a field testing kit for parasites. This has ensured that our design is as feasible and useful as possible. | |
| Meeting with Dr Martha Betson, Natural History Museum |
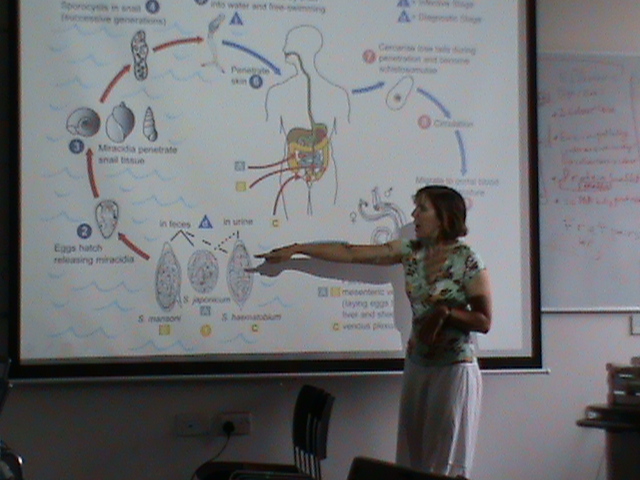
| Dr Martha Betson's research centres around the epidemiology of Schistosoma in Uganda where she works extensively in the field. Consequently, our meeting with Dr Betson gave us both a detailed overview of the biology of the schistosoma parasite, and valuable insights into the current efforts to control it.
From this meeting, we were able to identify that detection of schistosoma in the environment needs substantial research. Here's a photo of Dr Betson teaching us about the lifecycle of schistosoma: |
| Meeting with Professor Alan Fenwick and Dr Wendy Harrison of the
Schistosomiasis Control Initiative (SCI) |
| The SCI is based at the St Mary's Campus of Imperial College London and carries out research into NTDs, working with countries in sub-Saharan Africa to establish various disease control programmes.
The meeting was both informative and constructive, allowing us to shape our system so that it can be as useful as possible in a real world application. We discussed the sensitivity of our system, which would be a key issue in the development and implementation of the detection kit. It was suggested that sampling issues could be our biggest problem, because there are various factors that affect the population of cercariae in a particular volume of water. In addition to this, the lifespan of a cercaria is only around 24 hours, so any testing would need to be adapted to be statistically significant. We decided that using skin lipids, such as linoleic and linolenic acid, to attract cercariae to the testing device could be useful in terms of increasing the signal. It could also be possible to use a dipstick instead of using a fixed volume of water to test. This would mean that the test would take a longer time, but it would enable the detection of cercariae at much lower population densities. Dr Harrison suggested that we could use a visual signal to quantify the amount of cercariae present, for example by using a colour gradient similar to a pH indicator test. It was suggested that the sediment in the water may prevent one from seeing the colour change. However, we explained the modularity of our project, and how we could easily use a different output, such as smell. When discussing the possible uses for our detection kit, we found that organisations such as the CONTRAST project, which undertakes disease risk mapping in sub-Saharan Africa, could find our project very useful indeed. It may also be useful to have a test that distinguishes between different Schistosoma species. This could be done if the proteases released by each species had a slightly different amino acid recognition motif, which would define our linker sequence between the AIP and cell surface protein. We also wanted to know what Professor Fenwick and Dr Harrison's opinions were on praziquantel resistance. Resistance has not been observed, however a certain amount of tolerance to the drug has been noted. This occurs when a certain Schistosome is able to survive in the body after the drug has been administered. However, a higher dosage will easily kill the parasite and prevent the tolerant strain from spreading. Administration of praziquantel is not intended to reduce the transmission of schistosomiasis. Instead, it is hoped that by treating communities, the morbidity of the disease will decrease. It was noted that detection of the miracidia in stool would be a much more useful way to detect the parasite, because it would indicate whether or not a given community needs to be treated with praziquantel. We wanted to know if there were any other proteases that we might want to detect, in terms of NTDs. There is a protease which is released by Trypanosoma in the blood which could be used to diagnose Chagas disease. Currently, diagnosis of Chagas disease requires a lumbar puncture, which is hard to accomplish in resource-poor settings. |
| Meeting with Dr Julie Balen,
London School Of Hygiene and Tropical Medicine |
| Please watch the following video of our interview with Dr Balen:
align="center"| |
 "
"