Team:Washington/Gram Negative
From 2010.igem.org
(→New and Effective Killer of Gram-Negative Bacteria) |
|||
| Line 27: | Line 27: | ||
=New and Effective Killer of Gram-Negative Bacteria= | =New and Effective Killer of Gram-Negative Bacteria= | ||
[[Image: Washington Get away.jpg]] | [[Image: Washington Get away.jpg]] | ||
| - | + | It is becoming increasingly apparent that the old generation of small molecule antibiotics are becoming out-dated. Pathogens are continually evolving resistance to currently used antibiotics, and the discovery or modification of antibiotic treatments are slow to catch up. This continual evolution is causing the antibiotics to be less effective if not completely futile. Another problem with these antibiotics is that they do not differentiate between pathogenic and non-pathogenic bacteria; they kill both. There are many common diseases caused by gram-negative bacteria which inhabit the human gut, such as, but not limited to:''Vibrio cholerae''(cholera), ''Shigella'' (dysentary), and ''Salmonella'' (food poisoning). When these diseases are contracted antibiotics are most often given in hopes that they will kill the pathogenic bacteria. Quite often these antibiotics can cause a diverse range of side effects because they also end up killing other bacteria found naturally in the gut. Most of the bacteria in the gut are actually helpful. They aid the body in digestion, production of vitamins such as vitamin K, and competitively exclude pathogenic invaders. Both the problems of resistance and non-specificity could be lessened by an antibacterial agent that selectively kills pathogenic bacteria. This would limit the chance of the development of resistance by limiting exposure, and would drastically decrease damage to the helpful gut flora. The goal of this project is to turn the Tse2/Type VI secretion system, toxin/injection system, into a probiotic that specifically targets a pathogenic gram-negative bacteria and is activated only when that specific bacteria is present. | |
=The Type VI Secretion System= | =The Type VI Secretion System= | ||
Revision as of 00:09, 21 October 2010
New and Effective Killer of Gram-Negative Bacteria
 It is becoming increasingly apparent that the old generation of small molecule antibiotics are becoming out-dated. Pathogens are continually evolving resistance to currently used antibiotics, and the discovery or modification of antibiotic treatments are slow to catch up. This continual evolution is causing the antibiotics to be less effective if not completely futile. Another problem with these antibiotics is that they do not differentiate between pathogenic and non-pathogenic bacteria; they kill both. There are many common diseases caused by gram-negative bacteria which inhabit the human gut, such as, but not limited to:Vibrio cholerae(cholera), Shigella (dysentary), and Salmonella (food poisoning). When these diseases are contracted antibiotics are most often given in hopes that they will kill the pathogenic bacteria. Quite often these antibiotics can cause a diverse range of side effects because they also end up killing other bacteria found naturally in the gut. Most of the bacteria in the gut are actually helpful. They aid the body in digestion, production of vitamins such as vitamin K, and competitively exclude pathogenic invaders. Both the problems of resistance and non-specificity could be lessened by an antibacterial agent that selectively kills pathogenic bacteria. This would limit the chance of the development of resistance by limiting exposure, and would drastically decrease damage to the helpful gut flora. The goal of this project is to turn the Tse2/Type VI secretion system, toxin/injection system, into a probiotic that specifically targets a pathogenic gram-negative bacteria and is activated only when that specific bacteria is present.
It is becoming increasingly apparent that the old generation of small molecule antibiotics are becoming out-dated. Pathogens are continually evolving resistance to currently used antibiotics, and the discovery or modification of antibiotic treatments are slow to catch up. This continual evolution is causing the antibiotics to be less effective if not completely futile. Another problem with these antibiotics is that they do not differentiate between pathogenic and non-pathogenic bacteria; they kill both. There are many common diseases caused by gram-negative bacteria which inhabit the human gut, such as, but not limited to:Vibrio cholerae(cholera), Shigella (dysentary), and Salmonella (food poisoning). When these diseases are contracted antibiotics are most often given in hopes that they will kill the pathogenic bacteria. Quite often these antibiotics can cause a diverse range of side effects because they also end up killing other bacteria found naturally in the gut. Most of the bacteria in the gut are actually helpful. They aid the body in digestion, production of vitamins such as vitamin K, and competitively exclude pathogenic invaders. Both the problems of resistance and non-specificity could be lessened by an antibacterial agent that selectively kills pathogenic bacteria. This would limit the chance of the development of resistance by limiting exposure, and would drastically decrease damage to the helpful gut flora. The goal of this project is to turn the Tse2/Type VI secretion system, toxin/injection system, into a probiotic that specifically targets a pathogenic gram-negative bacteria and is activated only when that specific bacteria is present.
The Type VI Secretion System
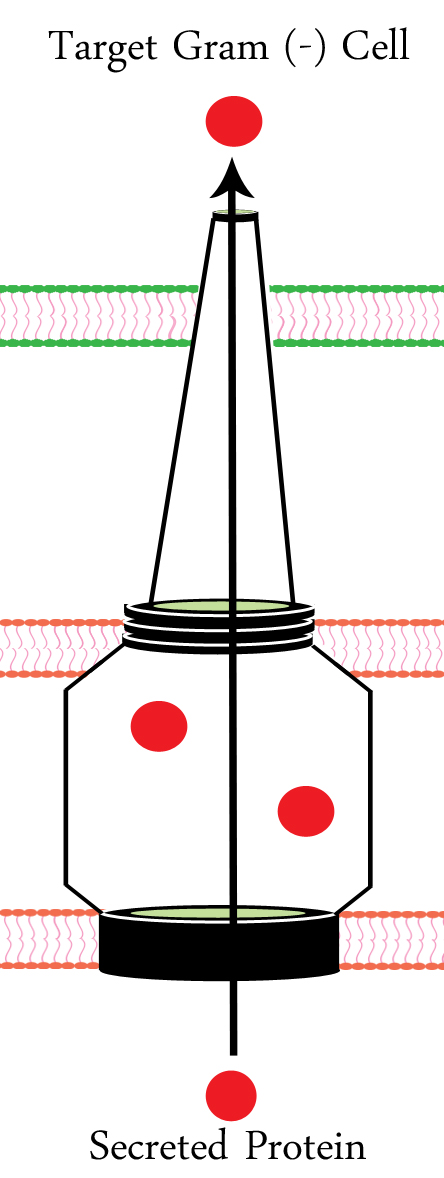
The T6SS (Type VI Secretion System) is an injection mechanism found in many (such as Pseudomonas aeruginosa), but not all gram-negative bacteria. E.Coli is one bacterial species that does not contain the T6SS. Since E.Coli is a common gram-negative bacteria found naturally in the gut it seemed only logical to move the T6SS into it. The T6SS acts much like a spear by physically puncturing the cell membrane. It also provides a channel through which proteins can be inserted into the punctured cell. The T6SS is physically incapable of puncturing the cell membrane of gram-positive bacteria, or the cell membrane of eukaryotic cells. This makes the T6SS a perfect candidate for a probiotic because it is unable to harm either human cells or helpful gram-positive bacteria.
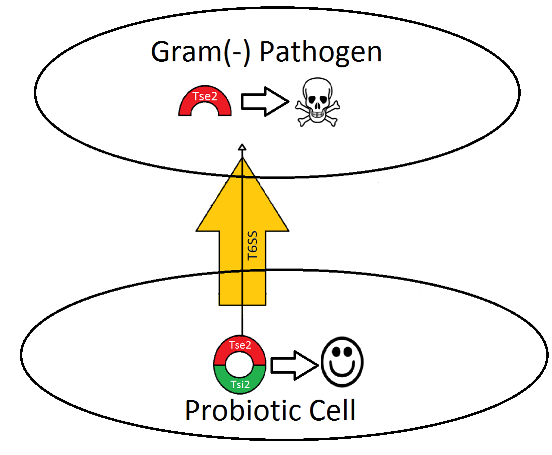
Tse2/ Tsi2 toxin/antitoxin system
In Pseudomonas aeruginosa, one of the major proteins secreted by the T6SS is the toxic protein Tse2. Normally, Tse2(red in figure 2) forms a complex with Tsi2(green in figure 2), a protein coexpressed with Tse2 that serves as an antitoxin. Before Tse2 is secreted into the target cell Tsi2 and Tse2 become unbound and Tse2 is secreted into the target cell by the T6SS. The presence of Tse2 unbound to Tsi2 causes the target cell to die. By controlling the activation of Tse2 and Tsi2 production and having it turn on only when a pathogen is present, we are able to help combat both problems of specificity and resistance.
 "
"